From Detecting Heart Disease to the Treatment of Osteoarthritis: The Latest Medical Discoveries of 2018
Posted on 2/27/18 by Suchita Chadha
We’re two months into 2018, but there already have been groundbreaking discoveries in the medical world that bring us closer to treatments for severe and often fatal conditions. Though they’re all in the early stages of research, the results provide an optimistic outlook for future developments.
Relationship Between Mutated Stem Cells and Heart Disease

Image captured from Human Anatomy Atlas.
When it comes to heart attacks and strokes, many people affected often display few or none of the common risk factors, such as high cholesterol and high blood pressure, smoking, diabetes, or family history. Clonal hematopoiesis of indeterminate potential (CHIP) is a newly discovered condition that appears to significantly increase the risk for a heart attack or stroke. CHIP is the accumulation of mutated stem cells in the bone marrow. These mutations are linked to leukemia—while they do not manifest into cancer, these stem cells grow faster and last longer than their normal counterparts. However, as an accidental discovery by multiple research groups investigating non-heart related conditions, the relationship between CHIP and heart disease is still being explored. At the moment, there does not seem to be any specific action that would reduce the risk of heart disease in patients with CHIP, but future research into the condition could help diagnose at-risk patients sooner and provide a recourse for prevention.
Artificial Intelligence Retinal Scan to Diagnose Heart Disease
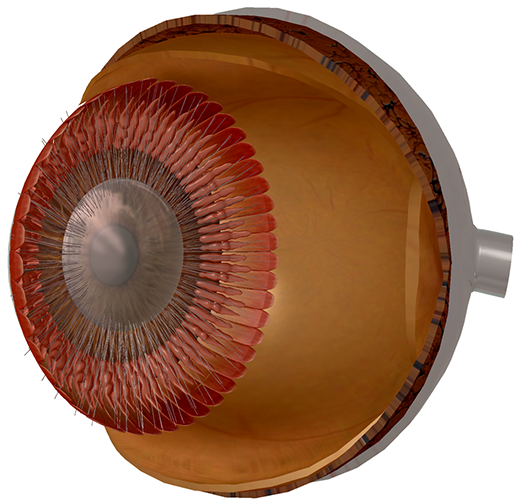
Image captured from Human Anatomy Atlas.
While the discovery of the relationship between CHIP and heart disease was accidental, Google researchers have been working toward using artificial intelligence (AI) technology that scans and interprets retinal images to detect a person’s risk of heart disease. Google’s deep learning algorithm was able to distinguish between smokers and non-smokers with a 71% success rate. It also predicted the systolic blood pressure in those with and without high blood pressure. The algorithm had 70% success rate in directly determining patients with the risk of a cardiovascular event within five years. This project is still in its early stages, with much more research and testing to be done; however, this breakthrough broadens the scope of using AI in the medical field.
Skin Cell Treatment for Multiple Sclerosis
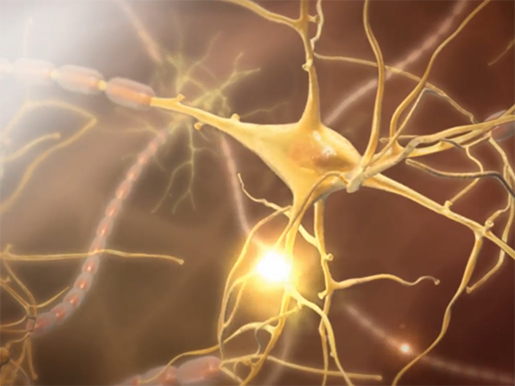
Image captured from Human Anatomy Atlas.
Scientists and researchers at the University of Cambridge, U.K., conducted a study on the use of a person’s own skin cells to repair nerve damage caused by multiple sclerosis (MS). A neurological disease in which the body’s immune system attacks the central nervous system, the cause of MS remains unknown, and there currently is no cure for the disease. In the study, skin cells were reprogrammed into neural stem cells (NSCs). Previously, NSCs had been discovered as a method of treatment for MS as they can transform into different kinds of cells in the central nervous system. However, since they can be taken only from embryos, they are not a sustainable means for ongoing treatment.
In contrast, skin cells are much easier to procure in large quantities, and the use of a person’s own cells reduces the risk of the immune system rejecting the NSCs as foreign bodies. When transplanted into the cerebrospinal fluid of mice, the reprogrammed skin cells—called induced neural stem cells (iNSCs)—were successful in reducing inflammation and repairing damage. Human clinical trials are still pending in the use of iNSCs from skin cells, but the study shows potential in creating a more effective treatment for MS.
Prevention & Treatment for Osteoarthritis
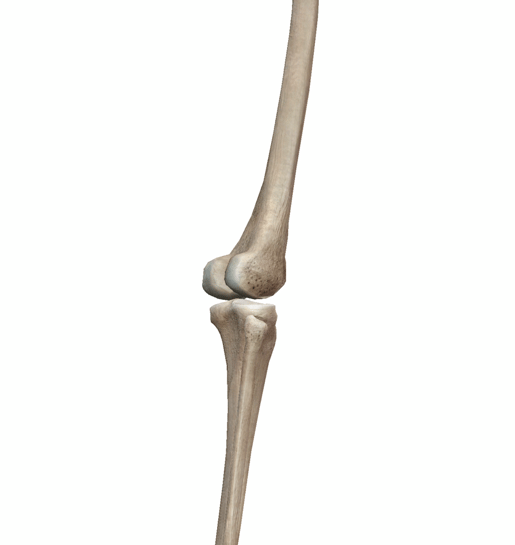
Image captured from Human Anatomy Atlas.
A recent study by The Scripps Research Institute (TSRI) found that a deficiency in FoxO proteins leads to the degeneration of joints at a younger age in addition to the failure to produce enough lubricin, a protein that protects joint cartilage by preventing friction. The FoxO protein comes from the Forkhead Box (FOX) family of transcription factors, which play a variety of important roles. In future studies, the researchers at TSRI plan to create molecules that increase FoxO levels and test them in experimental models of osteoarthritis.
Diagnosing Parkinson's Through Tears
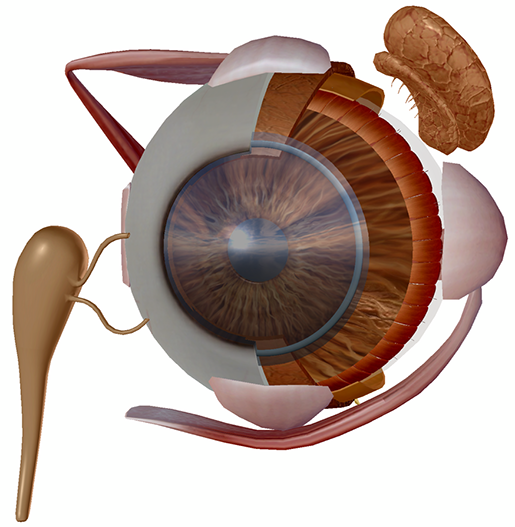
Image captured from Human Anatomy Atlas.
In a preliminary study by the Keck School of Medicine of the University of Southern California in Los Angeles, researchers found that determining protein levels released with tears could be a marker for Parkinson’s disease. The disease is a disorder in the central nervous system in which nerve cells don’t produce enough dopamine, primarily affecting movement. Since it impacts nerve function outside the brain, the study sought to examine the levels of four proteins produced in the lacrimal (tear) glands. Of the four proteins, the study found that there was less alpha-synuclein and more oligomeric alpha-synuclein in people with Parkinson’s. Since the symptoms of Parkinson’s may not appear for years after the disease has begun its course, the future prospects for this study are focused on investigating how early this marker can be discovered and testing the results with larger groups of people.
Be sure to subscribe to the Visible Body Blog for more anatomy awesomeness!
Are you a professor (or know someone who is)? We have awesome visuals and resources for your anatomy and physiology course! Learn more here.
Additional Sources:
- MedicalNewsToday & American Academy of Neurology
- MedicalNewsToday & The Scripps Research Institute
- MedicalNewsToday & University of Cambridge
- NYTimes



