Fascinating Medical Stories of 2020: COVID-19 Edition
Posted on 12/9/20 by Laura Snider
It probably won’t surprise you that much of this year’s medical news has concerned COVID-19—more than 59 million people have been infected and over 1.4 million people have died worldwide since the disease was declared a pandemic by the WHO in March. In one way or another, the pandemic has influenced everyone’s life this year.
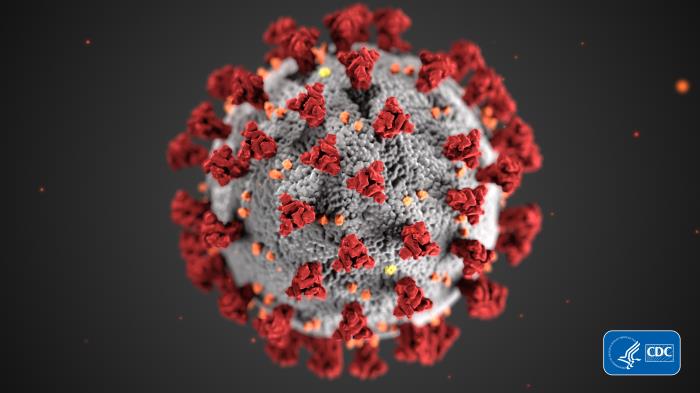 SARS-CoV-2, the virus that causes COVID-19. Image from the CDC’s Public Health Image Library.
SARS-CoV-2, the virus that causes COVID-19. Image from the CDC’s Public Health Image Library.
COVID is a devastating disease, and healthcare professionals and researchers have been working around the clock to mitigate the damage. Let’s take a look at just a few of the scientific advances and changes to medical care that the pandemic has led to over the past year.
1. Sequencing the SARS-Cov-2 virus and sharing data
In December 2019 and January 2020, reports of individuals suffering from severe respiratory infection in Wuhan, China, began circulating. By January 9, the World Health Organization and health authorities in China announced that the “viral pneumonia” cases they’d seen were caused by a novel coronavirus, 2019-nCoV. Only a few days later, the genome (genetic code) of the new virus was published online.
As the disease continued to spread, researchers around the world collected samples and used genomic sequencing to track new mutations and learn more about the proteins produced by the novel coronavirus. Initiatives like Nextstrain and GISAID have allowed scientists to collaborate and share data on a massive scale. According to the leader of the Nextstrain project, Professor Richard Neher, open access journals and online prepublishing of academic papers have also been key to the scientific community’s ability to rapidly share information and collaborate.
2. Increased access to telemedicine
Even before the pandemic, telemedicine was steadily increasing in popularity in the US. Telemedicine has many advantages, including expanding healthcare access for the elderly and people who live in rural areas, enabling easier follow-up care and monitoring of chronic conditions, and helping with triage in emergency settings.
When the need for social distancing limited access to hospitals and closed the physical offices of many private practices, telemedicine became a necessity for many people. The CDC reports that between January and March, “the number of telehealth visits increased by 50%, compared with the same period in 2019, with a 154% increase in visits noted in surveillance week 13 in 2020, compared with the same period in 2019.” In addition, ER visits were much less frequent during this portion of 2020 compared to 2019.
The CARES Act, passed in late March, supported the increasing need for telemedicine by including “improved provider payments for telehealth, allowance for providers to serve out-of-state patients, authorization for multiple types of providers to offer telehealth services, reduced or waived cost-sharing for patients, and permission for federally qualified health centers or rural health clinics to offer telehealth services.” Medicaid in many states also added telehealth visits as a covered benefit.
According to Stat News, COVID-19 accelerated the “inevitable telemedicine revolution” by nearly a decade, showing doctors and patients just how convenient it can be to interact with patients remotely, especially for quick check-ins and prescribing medications. So, while the pandemic-driven necessity of telemedicine will decline as vaccines for SARS-CoV-2 become available (more on that in a moment), some of the policies making it easier for doctors to see their patients remotely will hopefully remain.
3. New vaccine technology
If you’ve been reading the news in the last few weeks, you’ve most likely heard the (awesome) news that several vaccines for SARS-CoV-2, the virus that causes COVID-19, have proven effective in large-scale clinical trials. Two of those vaccine candidates, from Pfizer/BioNTech and Moderna, use a new(ish) method of immunization: the injection of mRNA. Let’s break down what this means and why it’s so cool. (Literally.)
Cells in the human body contain DNA, or deoxyribonucleic acid, which stores the instructions for how to make particular proteins out of amino acids.
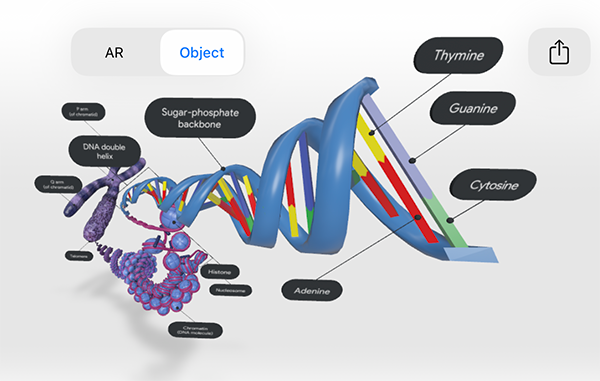 The DNA in a eukaryotic chromosome. Image from Visible Body's Biology Learn Site.
The DNA in a eukaryotic chromosome. Image from Visible Body's Biology Learn Site.
Our cells also contain RNA, or ribonucleic acid. One of RNA’s many roles in cells is to assist in protein synthesis via transcription and translation. Messenger RNA (mRNA) copies down information from the cell’s DNA and takes it to organelles called ribosomes so that protein assembly can begin.
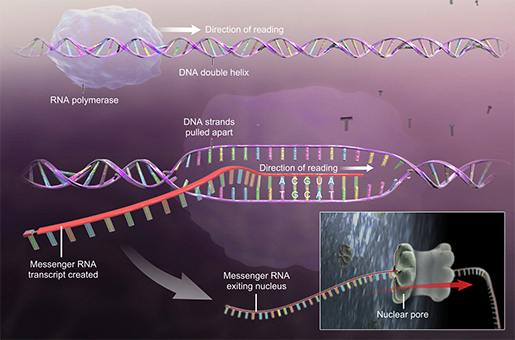
mRNA transcribing instructions for protein synthesis. Image from A&P.
The SARS-CoV-2 virus contains RNA, but not DNA. This means that when it infects cells in the human body, it hijacks them and gives them instructions to assemble viral proteins, which compromise our immune system and make us feel awful.
The way an mRNA vaccine works also capitalizes on protein synthesis. The particular sequence of mRNA used in the vaccine instructs cells at the injection site to produce one particular viral protein that the immune system can be “trained” to recognize but does not cause disease. Traditionally, vaccines have used dead or weakened forms of viruses, as well as proteins or other substances produced by viruses, to help the body learn to respond to those viruses without becoming ill.
4. Viable vaccine candidates
If (or when!) they are approved, the Pfizer and Moderna vaccines would be the first mRNA vaccines approved for use in humans—that’s very exciting on its own, and even better because a viable vaccine is what will allow life to return to normal.
This November, Pfizer and BioNTech’s SARS-CoV-2 vaccine was the first candidate reported to be successful following its Phase 3 clinical trial. The Pfizer vaccine proved 95% percent effective in preventing infection, even in older adults, which is excellent news. The success of Moderna’s vaccine in its Phase 3 trial was announced only a few days later—it was 94.5% effective in preventing infection.
The speed with which these vaccines have been developed is absolutely amazing. It shows that when the going gets tough, scientists get going!
However, distribution is going to be an issue, because it’s really hard to get a vaccine out to millions of people in a timely fashion. Vaccines, especially mRNA ones, require special storage conditions that can be hard to achieve in transit. Both the Pfizer and Moderna vaccines need to be stored at very low temperatures—negative 70 and negative 20 degrees Celsius, respectively—in order for the strands of mRNA to remain viable. If they get too warm, the mRNA molecules could break apart, rendering the vaccine ineffective.
While Pfizer has proposed special shipping containers that use dry ice to maintain the ultra-cold temperatures their vaccine needs, Moderna’s vaccine can be transported and stored using preexisting methods, since there are several vaccines for other diseases that require similar conditions.
Either way, it’s looking like these vaccines may soon receive emergency use authorization from the FDA. After that, the first doses will go to frontline healthcare workers and the most vulnerable members of the population. It will likely be a little while before doses can be administered to everyone, so we will need to keep following public health recommendations, such as social distancing and wearing masks, until then.
Be sure to subscribe to the Visible Body Blog for more anatomy awesomeness!
Are you an instructor? We have award-winning 3D products and resources for your anatomy and physiology course! Learn more here.



